Many people know that insulin resistance — also known as prediabetes and type 2 diabetes — is linked to obesity and heart disease. Few realize that insulin resistance is also associated with a less-discussed health problem. It’s one that affects women, even at young ages, and it’s called polycystic ovarian syndrome, or PCOS.
By understanding the relationship between PCOS and insulin resistance, you can prevent the damage caused by both conditions.
What is PCOS?
Women with PCOS produce higher-than-normal levels of male hormones, called androgens. The increase of androgens may cause some, or all, of the following symptoms:
- Irregular menstrual periods, typically very light periods and less frequent periods
- Acne
- Hair growth on the face and body
- Thinning hair on the head
- Ovarian cysts, which may cause pressure or pain in the pelvic area but are usually symptomless and are only discovered through ultrasound
- Infertility
PCOS is usually diagnosed based on blood tests that measure hormone levels. Sometimes, scans of the ovaries may be done to look for cysts, but visible cysts are not always present with PCOS.
PCOS is a common condition, with the Centers for Disease Control estimating that it affects 6% to 12% of reproductive age women in the US. Women who are overweight or obese are more likely to develop PCOS, but PCOS can occur in thin women as well. Research also suggests that PCOS has a genetic basis, so if you have a relative with PCOS or T2D, you may have a higher risk of developing PCOS.
Many women don’t realize they have PCOS for many months or even years, as the symptoms can be subtle. Girls and women can be diagnosed with PCOS in their teen years, but the symptoms are most commonly noticed when women are in their 20s or 30s.
PCOS and insulin resistance often go hand-in-hand
About 65 to 70% of women with PCOS have insulin resistance. Scientists believe that high levels of the hormone insulin are what cause male hormone levels to rise.
Insulin is a hormone that helps sugar enter the cells, through cells’ insulin receptors. People with insulin resistance need to produce more insulin than normal in order to process sugar. The risk of insulin resistance is especially high for women with PCOS who are also obese, at 70 to 80%.
If left unchecked, insulin resistance will progress to diabetes. Diabetes is diagnosed when blood sugar is above 200mg/dL, which can be identified with a HbA1c glucose test or, more preferably, an oral glucose test combined with insulin. It occurs when, even as the body produces excess insulin, the insulin receptors are functioning so poorly that they can’t take in adequate sugar for the cells. So it is not surprising that since women with PCOS have high rates of insulin resistance, they also have high rates of diabetes.
More than half of women with PCOS will be diagnosed with Type 2 diabetes by age 40. Studies show women with PCOS have four to nine times the diabetes risk compared to the general population. Women with PCOS who become pregnant are at a much higher risk of gestational diabetes first diagnosed during pregnancy, which can affect the pregnancy and the baby's health.
This is because the cell receptors are no longer properly responding to insulin — the vehicle for sugar to get into the cells. Signs of diabetes include:
- Frequent urination
- Extreme thirst and hunger
- Fatigue
- Numbness in the hands and feet
- Blurry vision
It’s important to remember that although there are classic signs of diabetes, the VAST majority of diabetics don’t notice any signs of symptoms in the early stages of the disease.
People with pre-diabetes may or may not have higher-than-normal blood sugar levels. Typically, they have high insulin levels because the body is adapting to a lower insulin response by producing more insulin.
Both pre-diabetes and diabetes often come with complications, so it’s really important to reduce insulin resistance to reduce the risk of complications, including vision loss, heart problems, and more.
Why is PCOS often paired with insulin resistance?
It’s theorized that insulin resistance contributes to PCOS, but PCOS, in turn, worsens insulin resistance.
As to how insulin resistance causes PCOS, many researchers think that chronically high insulin in the bloodstream encourages the ovaries to increase production of androgens. Insulin is a hormone, and it’s common that one hormone imbalance causes other hormones to go out of whack.
It’s important to add here that PCOS can occur for other reasons too, so insulin resistance is not the only pathway to developing PCOS.
Now, let’s get back to that cycle. Once PCOS occurs, the extra male hormones encourage fat to accumulate around the abdomen. You may have noticed that men are more likely to accumulate fat around the abdomen whereas women are more likely to accumulate fat at the hips. This due to the effects that male and female hormones have on the body.
As I’ve discussed before, fat cells around the abdominal organs are known for producing higher levels of proteins known as cytokines. These cytokines disrupt the normal functioning of insulin receptors and make them more resistant to insulin.
In other words, high levels of insulin worsens PCOS. As androgens increase with PCOS, that can lead to abdominal weight gain that further contributes insulin resistance.
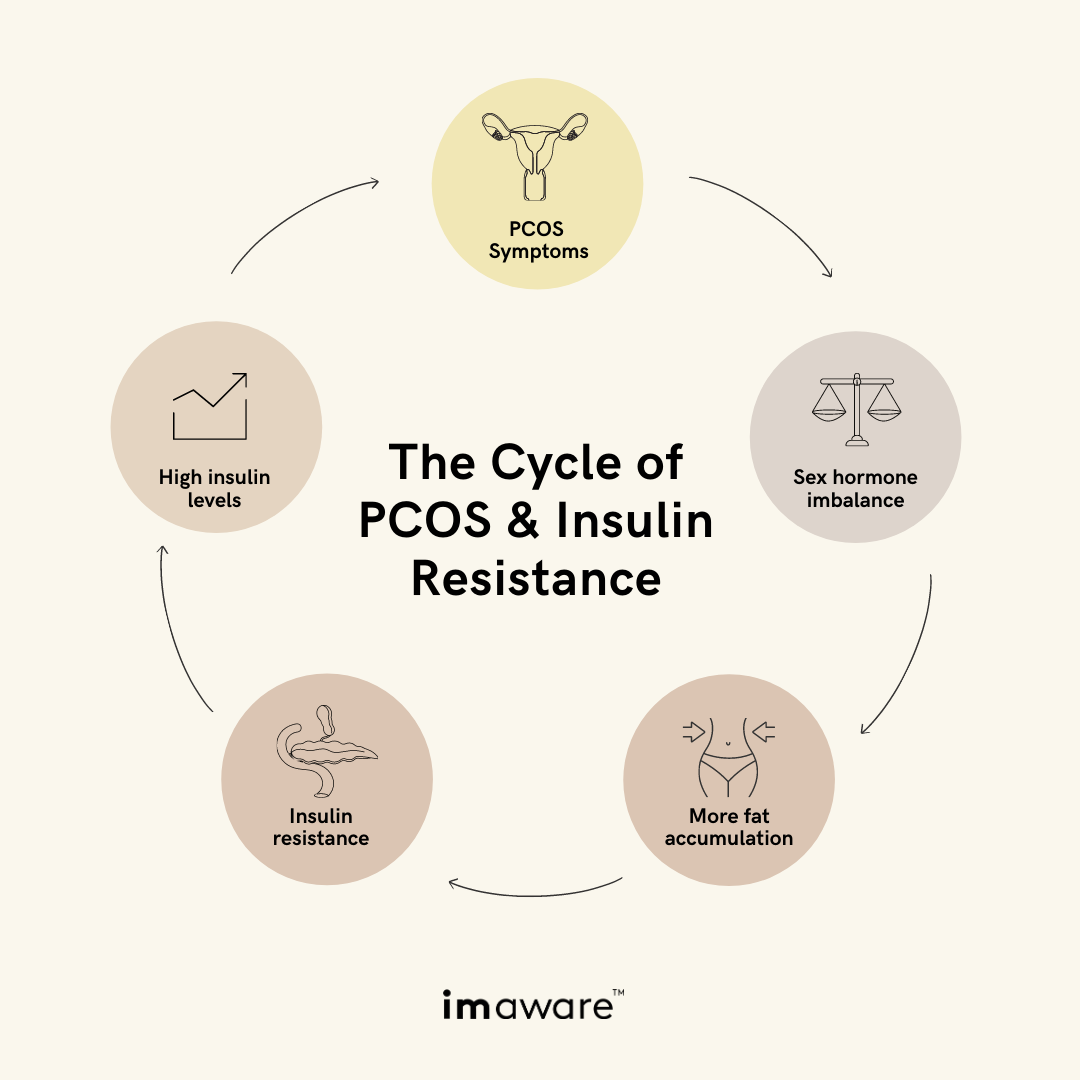
The dangerous cycle looks like this:
How to stop the vicious cycle of PCOS and insulin resistance
There is no cure for PCOS, only lifestyle modifications and medications to manage symptoms. But, the good news is that lifestyle changes that help with PCOS also help with insulin resistance. Lifestyle modification isn’t as easy as taking a pill. It’s about gradually improving your habits over time such as:
Regularly exercising
Exercise helps with both insulin resistance and PCOS. Exercise causes the insulin receptors on our muscle cells to take in sugars without requiring extra insulin production. Over time, this process makes the insulin receptors more sensitive to lower levels of insulin. That means the body responds by producing less insulin to process sugar. Lower insulin levels then leads to reduced androgen production, which helps with PCOS.
Adopting healthy eating habits
Healthy eating habits are also vital for women who have PCOS and insulin resistance, especially for those with a high BMI. The goal is sustained weight loss over time – keyword, sustained. Yo-yo dieting that causes us to lose and gain weight is very disruptive for our health and hormones.
By reducing abdominal fat, you’ll lower the level of cytokines produced by fat cells, which are harmful to insulin receptors. To put it another way, weight loss can help the insulin receptors work better and allow the pancreas to lower insulin production. This will reduce your levels of both insulin resistance and PCOS.
In addition, because insulin resistance reduces the body’s ability to break down carbs, it’s important to reduce carbs and simple sugars.
Reducing stress
It has been shown to help lower insulin resistance. Stress hormones encourage the liver to release stored sugars, leading to spikes in blood sugar and insulin.
The importance of testing for insulin resistance
If you suspect you may have PCOS, it’s recommended that you routinely take a blood glucose challenge test to measure whether you have insulin resistance. You should do this at least once a year, as well as with any weight gain or loss of 10 pounds or more.
By knowing your level of insulin resistance, you can see if it gets better over time with diet changes and exercise. You can also see how insulin resistance and PCOS are related for you as an individual. In other words, you can see if decreasing your body’s insulin resistance improves your PCOS symptoms.
PCOS and insulin resistance can have devastating effects, from infertility to vision damage to blood clots in the arteries. But PCOS and insulin resistance exist on a spectrum - you can have low levels of disease and high levels. Knowing where you stand is the first step to taking control of your health.














.svg)




